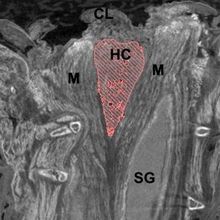
A light micrograph of a section of fetal ovary shows primordial follicles (light pink ovals) with oocytes (dark pink spots) that have already begun to mature into fertilizable eggs. But the process won’t be complete for decades, during which time mistakes in chromosome division can occur.© TISSUEPIX/SCIENCE SOURCE
A light micrograph of a section of fetal ovary shows primordial follicles (light pink ovals) with oocytes (dark pink spots) that have already begun to mature into fertilizable eggs. But the process won’t be complete for decades, during which time mistakes in chromosome division can occur.© TISSUEPIX/SCIENCE SOURCE
Up to a quarter of pregnancies are not carried to term; oftentimes an embryo is aborted by the body before a woman even knows she’s pregnant. The most common cause of miscarriage is egg aneuploidy—the oocyte contains too many or too few chromosomes. Aneuploidy is thus the leading genetic cause of infertility, and those embryos that are not miscarried can result in children with developmental disorders, such as Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), and Turner syndrome (monosomy X).
The life of an oocyte begins during female fetal development but does not finish for decades, providing multiple windows...
For more than 80 years, the scientific community has known that the incidence of Down syndrome births increases with maternal age and that female fertility rapidly declines after the age of 35.1 These concerns can be bypassed by the use of donor eggs from younger women, however, suggesting that the eggs of older women are the source of the reproductive decline, not the mother’s reproductive system itself. Sure enough, up to 20 percent of eggs in healthy females may be aneuploid, and this number increases with age. But despite the ubiquity of egg aneuploidy, the cellular and genetic reasons for the phenomenon are poorly understood.
We now know that the multistage process of meiosis that forms a woman’s eggs is highly error prone.2 While germ-line meiosis in males initiates at puberty and provides a fresh supply of haploid sperm cells until death, the life of an oocyte begins during female fetal development but does not finish for decades, providing multiple windows of opportunity for problems that compromise egg quality. And in the past two years, clinicians and basic scientists have started conducting analyses of human oocytes to get at the molecular details of this pervasive problem. Thanks to technical advances, such as genome-wide recombination mapping and high-resolution, live-cell imaging, we now have a clearer picture of how chromosomes behave during meiosis.
Once scientists understand the basic machinery that controls meiosis, they can develop appropriate diagnostics and interventions to help women achieve pregnancies with egg cells that have properly apportioned chromosomes. Currently, one in six couples is infertile, and about half of those cases are due to abnormalities on the female side. And as the average age at which a woman experiences her first pregnancy increases in the U.S. and other developed countries—in some nations, that age has reached 30—the challenges of aneuploidy will only become more common.
Divvying up the genome
 ASYMMETRIC DIVISION: Just before ovulation, the first cell division of meiosis yields a large oocyte (green) and much smaller polar body (yellow).© PROF. P.M. MOTTA/UNIV. “La Sapienza”, ROME/SCIENCE SOURCEDuring female fetal development, the primordial germ cells that give rise to oocytes replicate their full diploid complement of DNA, with each chromosome forming two sister chromatids joined along the arms and centromeres by a protein complex known as cohesin. Homologous chromosomes then pair with each other and exchange bits of DNA through homologous recombination. The process involves breaking the chromosomes and swapping bits of DNA between nonsister chromatids of a homologous pair (homologs). During the swap, termed crossing over, linkages called chiasmata form between homologs and are maintained until the onset of anaphase I several decades later, when the chromosomes are pulled apart before division into two daughter cells. This marks the completion of the first stage of meiosis (Meiosis I). If chiasmata fail to form, the chromosomes may separate improperly, a phenomenon known as nondisjunction. (See illustration below and “Picturing Inheritance, 1916.”) Most cases of trisomy 21 are due to maternal nondisjunction.
ASYMMETRIC DIVISION: Just before ovulation, the first cell division of meiosis yields a large oocyte (green) and much smaller polar body (yellow).© PROF. P.M. MOTTA/UNIV. “La Sapienza”, ROME/SCIENCE SOURCEDuring female fetal development, the primordial germ cells that give rise to oocytes replicate their full diploid complement of DNA, with each chromosome forming two sister chromatids joined along the arms and centromeres by a protein complex known as cohesin. Homologous chromosomes then pair with each other and exchange bits of DNA through homologous recombination. The process involves breaking the chromosomes and swapping bits of DNA between nonsister chromatids of a homologous pair (homologs). During the swap, termed crossing over, linkages called chiasmata form between homologs and are maintained until the onset of anaphase I several decades later, when the chromosomes are pulled apart before division into two daughter cells. This marks the completion of the first stage of meiosis (Meiosis I). If chiasmata fail to form, the chromosomes may separate improperly, a phenomenon known as nondisjunction. (See illustration below and “Picturing Inheritance, 1916.”) Most cases of trisomy 21 are due to maternal nondisjunction.
Last year, Christian Ottolini in Eva Hoffman’s laboratory at the University of Kent in the U.K. and colleagues generated genome-wide recombination maps, dubbed “MeioMaps,” and found evidence that properly functioning recombination is indeed protective against chromosome segregation errors in human oocytes. Using single nucleotide polymorphism (SNP) arrays with some 300,000 genetic markers, the researchers pinpointed the sites of recombination in 13 human oocytes and their associated polar bodies—the nonfunctioning cells produced during meiosis that do not become the mature egg—as well as 10 embryo–polar body sets from patients undergoing in vitro fertilization (IVF). Notably, this is the first time researchers have assessed all the products from a complete meiosis. In addition, the researchers performed preimplantation genetic diagnosis of 29 embryos to diagnose aneuploidy. While the number of recombination events were highly variable between samples, they tended to decrease with age. And oocytes that underwent less recombination were more likely to be aneuploid.3
Nondisjunction is not the only way to get eggs with an incorrect number of chromosomes. In fact, some data indicate that a more-frequent cause of aneuploidy is the premature separation of sister chromatids (PSSC).4,5 Under normal conditions, cohesin is deposited along the length of chromosomes during premeiotic DNA replication to hold sister chromatids together. At the onset of anaphase during meiosis I, cohesin is cleaved along the chromosome arms, but it is protected at sister centromeres by a protein called shugoshin to ensure that sister chromatids remain together as homologs segregate. During anaphase of meiosis II, the remaining cohesin is cleaved, allowing sister chromatid separation and the formation of four fully haploid daughter cells. Therefore, to ensure proper sister chromatid associations throughout oocyte maturation, cohesin proteins laid down during fetal development must still be functional decades later.6 If cohesin is lost or rendered dysfunctional at any point along the way, the sister chromatids can be pulled into different daughter cells prematurely.
Sure enough, as my colleagues and I as well as other groups have found, cohesin levels are reduced and sister chromatid centromeres begin to separate prematurely in oocytes from aged mice.7,8,9 Similarly, the distance between sister chromatids in human oocytes increases with maternal age and aneuploidy rates go up.10,11 These observations support the hypothesis that exhaustion of cohesin can lead to increased PSSC in human eggs.
Additionally, while in mice and other model organisms sister chromatid kinetochores—the two centromeric protein complexes that attach to the spindle microtubules extending from the cell’s poles during meiosis—are fused together, recent research suggests that the same may not be true of chromosomes in human eggs. Last year, two independent groups used high-resolution imaging to examine the geometry of the sister-chromatid kinetochores in human oocytes harvested for IVF and found that they were not fused, and thus did not act as a single unit as they do in mice and other organisms, where they serve as further insurance that both chromatids end up in the same daughter cell following the first meiotic division.12,13 The distance between sister chromatid kinetochores in human oocytes increases with maternal age, but kinetochore separation is also frequently observed in younger women, possibly contributing to the fact that even young women can have high rates of meiotic aneuploidy.14,15 (See “In the Genes” below.)
But high rates of PSSC do not rule out a role for recombination defects in aneuploidy. In 2006, Beth Rockmill, then in Shirleen Roeder’s lab at Yale University, and colleagues observed wild-type yeast strains engineered to harbor an extra copy of chromosome 3 containing selectable markers so that they could easily detect PSSC. After dissecting 1,300 tetrad spores—the equivalent of a mammalian egg and its three polar bodies—the researchers found a correlation between PSSC and crossovers that occurred close to the centromere, suggesting that where along their length homologous chromosomes recombine is important. If the crossover is too close to the centromere, it may interfere with sister chromatid cohesion, causing the sister chromatids to dissociate.16 Ottolini and collaborators also found that some chromosomes in human eggs failed to suppress crossovers at or close to centromeres—consistent with the team’s observations of elevated PSSC.
 MEIOTIC MYSTERIES: Meiosis in human females takes place over decades. At any point in this process, an incorrect number of chromosomes can be transferred to daughter cells, resulting in aneuploid gametes, the most common cause of miscarriage and the root of certain developmental disorders, such as Down syndrome.
MEIOTIC MYSTERIES: Meiosis in human females takes place over decades. At any point in this process, an incorrect number of chromosomes can be transferred to daughter cells, resulting in aneuploid gametes, the most common cause of miscarriage and the root of certain developmental disorders, such as Down syndrome.
See full infographic: WEB | PDF© 2016 MICA DURAN
All of these missegregation scenarios are chromosome-centric. What is missing from these pictures, however, is the behavior of the microtubules that connect the chromosomes to the spindle poles on opposite sides of the cell. Even if sister chromatids do separate prematurely, they may not segregate improperly if the microtubules hook up as they would if the chromatids were still attached. But if these connections are not correct, chromosomes are at risk of ending up in the wrong daughter cell. The attachment of sister kinetochores to microtubule fibers from opposite poles during meiosis I, for example, could cause sister chromatids to split up. As the distance between sister chromatids increases with maternal age, the risk of such aberrant microtubule attachment also likely increases.
By visualizing 100 human oocytes as they underwent spindle formation during meiosis I, Zuzana Holubcová in Melina Schuh’s laboratory at the Medical Research Council in Cambridge, U.K., and colleagues observed several abnormalities in building the spindle.17 In some cases, the spindle structure was unstable and would either lack any poles or become multipolar. The researchers also noted chromosome segregation problems such as lagging chromosomes that would remain in the center of the spindle during anaphase I. They hypothesized that these lagging chromosomes resulted from errors in how the microtubules attached. Taking a snapshot of the microtubule connections, they found that 20 percent of sister chromatid kinetochores attached to both poles instead of a single pole. In mice, such attachment is a trial-and-error process in which aberrant connections are normally fixed. If human oocytes are inefficient at correcting such attachment errors, it could explain the high rate of chromosome missegregation during the formation of human eggs.
Additionally, all of the human oocytes Holubcová tracked lacked microtubule-organizing centers that help coordinate spindle assembly in mouse oocytes. Instead, chromosomes initiated microtubule growth. Moreover, the researchers discovered that human oocytes took an unusually long time to build the spindle—a whopping 16 hours, compared to just 5 hours in mouse oocytes and the 30 minutes it takes cells to build spindles for mitotic division. Such inefficient spindle formation could favor incorrect attachments that can lead to aneuploidy. Given the importance of microtubule attachments for proper chromosome segregation in human oocyte development, studying oocyte spindle biology will be critical to understanding why meiosis I is so error prone.
A closer look
Surprisingly, improper chromosome segregation doesn’t always lead to aneuploid oocytes. Ottolini’s team observed, for example, that some oocytes that had experienced PSSC still contained the proper number of chromosomes at the end of meiosis II. Specifically, these oocytes appeared to have completed meiosis backwards, separating sister chromatids in meiosis I and homologous chromosomes in meiosis II, as evidenced by the fact that their first polar bodies (formed during meiosis I) contained a pair of homologous chromosomes, each with just one sister chromatid. During the second meiotic division, then, the oocytes segregated those homologous chromatid pairs, resulting in a euploid cell, or one with a normal chromosome number. This phenomenon, which the authors termed “reverse segregation,” brings into question how ordered chromosome segregation actually is in human oocytes.
Only once scientists understand the basic machinery that controls meiosis can they develop appropriate diagnostics and interventions to help women achieve pregnancies with egg cells that have properly apportioned chromosomes.
A similar phenomenon could also result when paired homologous chromosomes, or bivalents, separate prematurely. In the 1990s, Roslyn Angell at the University of Edinburgh examined 200 discarded oocytes from patients undergoing IVF and observed 61 cases of lone homologs (univalents) that had apparently separated precociously during metaphase of meiosis I, prior to the first meiotic cell division.18,19 Last year, using live, high-resolution confocal microscopy to track individual kinetochores, Yogo Sakakibara in Tomoya Kitajima’s laboratory and colleagues at the RIKEN Center for Developmental Biology in Kobe, Japan, documented the same phenomenon in oocytes from young and old mice: homolog kinetochores were sometimes farther apart than normal, and this often led to univalent formation.20
The resulting univalents had one of three fates during meiosis I, two of which involve unbalanced segregation: both chromatids of one univalent could segregate into one daughter cell, while the chromatids of the other homolog were separated, or all four chromatids of the two univalents could end up in the same daughter cell. Most of the time, however, the segregation was balanced, where the two sister chromatids of each homolog segregated into separate daughter cells. The resulting egg was euploid but with one sister chromatid from each homolog instead of both chromatids from a single homolog—just like the reverse segregation patterns observed by Ottolini’s team. (See illustration above.)
Sakakibara and colleagues also examined three human oocytes from donors over the age of 35 and again observed univalents prior to meiosis I segregation, suggesting that this separation of homologs may contribute to high rates of egg aneuploidy. But because a balanced division of the resulting univalents would result in a euploid egg, a chromosome analysis without watching the chromosome behavior would fail to detect any issue. Only through the power of live imaging can researchers detect improper, yet balanced, chromosome segregation.
Because these embryos are euploid, it is not known if they are developmentally equivalent to those derived from classical meiotic segregation.21 Perhaps selection of these euploid embryos for transfer could help explain the low success rates of IVF procedures, in which fertilized eggs are screened for aneuploidy and other chromosomal abnormalities before being transplanted into the host uterus. If such reverse segregation is detrimental to the fetus, IVF screens must sample both embryos and polar bodies after fertilization to identify all cases where meiosis may have gone awry.
A grain of salt
While the study of oocytes retrieved from IVF clinics has greatly improved our understanding of mistakes that can occur during meiosis, the results must be interpreted with caution. Most of the patients have undergone hormonal stimulation to increase the number of oocytes retrieved, possibly recruiting oocytes of poorer quality. Moreover, eggs that successfully complete meiosis I are fertilized and developed into embryos, leaving those oocytes that have not yet completed meiosis I to be used for these types of studies. Therefore, it is possible that these discarded oocytes are not representative of how a healthy oocyte would behave.
Currently, most US states and other countries do not allow financial compensation to women to donate their oocytes for research. It is therefore rare that one would volunteer to undergo an invasive process for the sake of scientific advancement, thereby limiting the oocytes used in experiments to those from women undergoing IVF.
In addition to the remaining questions about how chromosomes in normal human oocytes (mis)behave, we are also left with trying to understand why. What molecular players are deficient in human oocytes compared to other organisms such as mice that have lower rates of aneuploidy? Can methods of gamete selection that aim to fertilize only the eggs that did everything right during meiosis I be improved? And is it possible to develop interventions to correct this error-prone process when patients are undergoing IVF?
Answering these questions will be essential for improving IVF outcomes. Hopefully, by coupling these observational experiments using human oocytes with genetic and cellular biological experiments that can be conducted in model systems, researchers in the field of human reproductive biology will soon solve these mysteries.
Karen Schindler is an assistant professor who studies reproductive biology in the Department of Genetics at Rutgers, The State University of New Jersey.
|
IN THE GENES Although maternal age is clearly associated with the incidence of aneuploidy, it does not explain why some reproductively young women (<35 years of age) have higher than average levels of aneuploidy. Some population-based studies point to genetics as the missing link. For example, marriages between close relatives are associated with increased aneuploidy among children in specific populations. In 1970, an estimated 50 percent of all marriages among native Kuwaitis occurred between close family members, and 40 percent of non-native Kuwaitis living in the country were in familial marriages (Clin Genet, 27:483-86, 1985). Data from the 11,614 births that occurred that year in the Kuwait Obstetric Hospital supported the effects of increased maternal age, but also pointed to close kinship between the parents as causing an increase in the incidence of children born with Down syndrome. Bedouin Kuwaitis, who have higher rates of consanguineous marriages than urban Kuwaitis, had nearly double the risk of having a child with the disorder (3/1,000 births, compared with 1.6/1,000 births). Analyses of Down syndrome in the U.S. between 1983 and 1990 have also linked genetics to rates of the disorder. Data from 17 state surveillance programs revealed higher rates of Down syndrome for Hispanic populations (1.8/1,000 births) than for white (0.92/1,000 births) and black populations (0.72/1,000 births), even when controlling for maternal age. The US Centers for Disease Control and Prevention blamed these discrepancies on the differential use of prenatal diagnostics, but this trend for Hispanic mothers was also identified in South American countries, where access to these services is more equal: in a remote hospital in Chile between 1997 and 2003, the prevalence of Down syndrome was 2.96/1,000 live births. These studies, and many others, support the hypothesis that some women are genetically predisposed to producing aneuploid gametes, even at a young age.
With the advent of embryo screening in IVF clinics, together with the decreasing costs of next-generation sequencing, it is easy to imagine that an evaluation of the genomes of patients who produce more or fewer aneuploid embryos could identify causal gene variants. In a genome-wide analysis of single nucleotide polymorphisms (SNPs) in 2,362 unrelated mothers, for example, researchers identified a region of chromosome 4 that is associated with a mistake in the first mitotic division after fertilization (Science, 348:235-38, 2015). Of the many genes contained in this region of chromosome 4, polo-like kinase 4 (PLK4) stands out as possibly important for maintaining the correct chromosome number in the developing embryo, as it is known to regulate spindle formation in other cell types. This functional connection has yet to be tested, however, and until more studies are conducted, the scientific community remains largely in the dark about the genes that underlie gamete quality. |
References
- L.S. Penrose, “The relative effects of paternal and maternal age in mongolism,” J Genet, 27:219-24, 1933.
- T. Hassold, P. Hunt, “To err (meiotically) is human: The genesis of human aneuploidy,” Nature Rev Genet, 2:280-91, 2001.
- C.S. Ottolini et al., “Genome-wide maps of recombination and chromosome segregation in human oocytes and embryos show selection for maternal recombination rates,” Nature Genet, 47:727-35, 2015.
- F. Pellestor et al., “Maternal aging and chromosomal abnormalities: New data drawn from in vitro unfertilized human oocytes,” Hum Genet, 112:195-203, 2003.
- R. Garcia-Cruz et al., “Dynamics of cohesin proteins REC8, STAG3, SMC1 beta and SMC3 are consistent with a role in sister chromatid cohesion during meiosis in human oocytes,” Hum Reprod, 25:2316-27, 2010.
- S. Burkhardt et al., “Chromosome cohesion established by rec8-cohesin in fetal oocytes is maintained without detectable turnover in oocytes arrested for months in mice,” Curr Biol, 26:678-85, 2016.
- L.M. Lister et al., “Age-related meiotic segregation errors in mammalian oocytes are preceded by depletion of cohesin and Sgo2,” Curr Biol, 20:1511-21, 2010.
- T. Chiang et al., “Evidence that weakened centromere cohesion is a leading cause of age-related aneuploidy in oocytes,” Curr Biol, 20:1522-28, 2010.
- K. Tachibana-Konwalski et al., “Rec8-containing cohesin maintains bivalents without turnover during the growing phase of mouse oocytes,” Genes Dev, 24:2505-16, 2010.
- F.E. Duncan et al., “Chromosome cohesion decreases in human eggs with advanced maternal age,” Aging Cell, 11:1121-24, 2012.
- M. Tsutsumi et al., “Age-related decrease of meiotic cohesins in human oocytes,” PLOS ONE, 9:e96710, 2014.
- J. Patel et al., “Unique geometry of sister kinetochores in human oocytes during meiosis I may explain maternal age-associated increases in chromosomal abnormalities,” Biology Open, doi:10.1242/bio.016394, 2015.
- A.P. Zielinska et al., “Sister kinetochore splitting and precocious disintegration of bivalents could explain the maternal age effect,” eLife, 4:e11389, 2015.
- F. Pacchierotti et al., “Gender effects on the incidence of aneuploidy in mammalian germ cells,” Environ Res, 104:46-69, 2007.
- A. Obradors et al., “Whole-chromosome aneuploidy analysis in human oocytes: focus on comparative genomic hybridization,” Cytogenet Genome Res, 133:119-26, 2011.
- L. Jessop et al., “Meiotic chromosome synapsis-promoting proteins antagonize the anti-crossover activity of sgs1,” PLOS Genet, 2:e155, 2006.
- Z. Holubcová et al., “Error-prone chromosome-mediated spindle assembly favors chromosome segregation defects in human oocytes,” Science, 348:1143-47, 2015.
- R.R. Angell, “Predivision in human oocytes at meiosis I: A mechanism for trisomy formation in man,” Hum Genet, 86:383-87, 1991.
- R. Angell, “First-meiotic-division nondisjunction in human oocytes,” Am J Hum Genet, 61:23-32, 1997.
- Y. Sakakibara et al., “Bivalent separation into univalents precedes age-related meiosis I errors in oocytes,” Nature Commun, 6:7550, 2015.
- E.J. Forman et al., “Oocyte vitrification does not increase the risk of embryonic aneuploidy or diminish the implantation potential of blastocysts created after intracytoplasmic sperm injection: A novel, paired randomized controlled trial using DNA fingerprinting,” Fertil Steril, 98:644-49, 2012.
Interested in reading more?